

May = Osteoporosis Awareness Month
Osteoporosis is the most common bone disorder in America, occurring in 50 percent of women, leading to 1.5 million fractures each year (Office of the Surgeon General 2004). Spinal compression fractures may cause a deformed spine, height loss, pain, appetite loss, heartburn, bloating, and difficulty breathing.
You may not realize that your bones are constantly changing. If you gain weight, your bones need to become stronger to support the load. For instance, if you start a couch-to-5K training program, your muscles will create a positive load on your bones, molding them and creating better stability, literally increasing bone density.
Our bones start out as cartilage. Then osteoblasts, which are bone builders, help to change cartilage to bone when we are young, and they continue to remodel our bones as we age. They lay the matrix that makes up our bones. This matrix contains collagen, calcium, and phosphates (called hydroxyapatite).
Calcium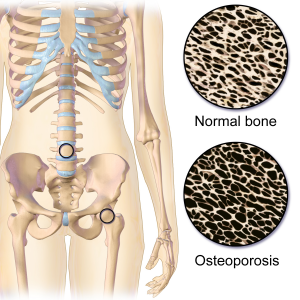
Women who have had a hysterectomy or are postmenopausal are at higher risk for osteoporosis. This is specifically because of the resulting hormone decline. Estrogens keep osteoclasts (bone breakers) at bay. When estrogen is low, osteoclast activity can increase. Steroid and reflux medications can also contribute to bone loss, because they reduce hormone production and nutrient absorption, respectively.
Additional risk factors for osteoporosis include being older, being a woman, having a thin stature, being of Caucasian and Asian ethnicity, not exercising, alcoholism, smoking, crash dieting, eating disorders, and nutritional deficiencies like calcium and Vitamin D.
Osteoporosis is often detected by a dual-energy x-ray absorptiometry (DEXA) scan, also called a bone density scan. A T-score of 0 means your bone mineral density (BMD) is equal to the norm for a healthy young adult. Osteopenia occurs when BMD is between 1 and 2.5 standard deviations below peak young adult BMD (T-score between -1 to -2.5). Osteoporosis occurs when BMD ≥ 2.5 standard deviations below normal (T-score is -2.5 or lower).
If you had an unusual fracture unexpectedly at a young age, it is beneficial to have your BMD tested. I’ve seen women in their twenties and thirties already with osteoporosis, some from low hormone levels if their period cycles have been irregular of stopped. Also, every postmenopausal woman should have a bone density test to assess her baseline to know if she is already osteopenic or osteoporotic. Some believe that fracture risk could be as high as 20 percent for those with osteoporosis. Fractures increase the risk of death. Several studies have shown that an osteoporosis fracture in men or women increases the risk of dying within five to ten years following the injury compared to the normal population (Bluic et al. 2009). To reduce this risk, those with bone density issues should be treated or better yet bone density issues should be…prevented!
Establishing a high peak bone mass (PBM) by the age of twenty may be one of the most important factors in maintaining strong bones in your elderly years. Having osteoporosis increases fracture risk, increasing risk of death. The mortality rate after a hip fracture can range from 14 to 58 percent (Studd et al. 1990)!
PBM is best achieved with regular weight-bearing exercises which force you to work against gravity. These exercises include:
- Hiking
- Jogging
- Climbing stairs
- Playing tennis
- Dancing
- Weight lifting
Exercise promotes blood flow, which helps with healing injuries and maintaining weight. Maintaining a healthy weight is very important, since being overweight adds additional pressure to your joints and back.
Caffeine and soft drinks are natural diuretics that rob your body of essential bone-building nutrients. Additionally, carbonated beverages will leach minerals from your bones. Studies have shown that increased carbonated soft drink consumption by young girls reduces bone mass density (BMD) and dramatically increases fracture risk (Samano et al. 2013). And, as I discuss further in chapter 4 of my book Your Longevity Blueprint, drugs also induce micronutrient deficiencies.
Optimizing hormones can greatly benefit bone density. Replacing estrogen, progesterone, and testosterone in women—and testosterone in men—will help reduce bone loss, and can even help with cartilage renewal. I’ve seen both female and male patients in my functional medicine practice with osteoporosis or similar conditions who experience joint pain reduction and BMD improvement using natural hormone replacement therapy. However, testosterone replacement via pellet therapy, discussed later in chapter 6, has shown the most dramatic rise in BMD, as great as 8.3 percent (Studd et al. 1990). I have not seen any drug or lifestyle change improve BMD to this degree.
There are several nutrients that can assist with bone and joint health: Calcium, Vitamin D, Magnesium, K2, and Strontium.
Most individuals are aware that our bones are composed of calcium and phosphorus. Yes, we need to consume calcium from our diet or from supplements, but your bones need more than calcium.
Vitamin D is mentioned in many chapters in my book. It helps your body absorb calcium and phosphorus from the food you eat, and it is important for bone remodeling by osteoblasts and osteoclasts.
Without enough magnesium, calcium can collect in the wrong places in the soft tissues and cause arthritis. Therefore, magnesium is just as important as calcium. Two-thirds of the magnesium in our bodies is located within the bones (Castiglioni 2013). Magnesium is very important for osteoporosis, and “represents a helpful intervention to maintain bone integrity” (Castiglioni 2013). A commonly recommended ratio of magnesium to calcium is 2 to 1, although most women consume less magnesium than that. Magnesium activates enzymes involved in forming new calcium crystals, and helps with calcium absorption, as well as converting vitamin D to its active form. If you’ve had challenges improving your vitamin D level despite high dosing, it may be because you are low in magnesium.
A much-overlooked nutrient for bone health is vitamin K. Low levels of vitamin K2 are directly related to reduced BMD. K2 helps bind calcium into the bone. Vitamin K is a primary cofactor in absorption of calcium into bone. It synergistically works with vitamin D3 to improve calcium absorption. Think of vitamin D as the doorman opening the door for calcium to enter the blood stream. Vitamin K is the usher that takes calcium from the lobby and directs it to its appropriate seat in the bone matrix. We carry vitamin D3 products in both liquid and capsule form, with and without K2.
Strontium is another mineral I use in my functional medicine practice for my patients with osteopenia and osteoporosis. Randomized, double blind, placebo controlled clinical trials show that strontium ranelate at a dose of 1 g/day significantly increases bone mineral density compared to placebos, and reduces the incidence of fractures (Reginster et al. 2002). Strontium has previously demonstrated its effectiveness in several different trials (PREVOS, STRATOS, TROPOS, and SOTO). Strontium stimulates new bone growth by helping bone turnover. How does it work? It promotes osteoblastic activity and reduces osteoclastic activity. Our strontium Longevity Blueprint (LB) product is called Strontium Chelate.
Looking for 1 well rounded bone building product with all the nutrients I’ve mentioned? Another one of our LB products, Bone Support, is a bone-building pack we offer to our patients with bone density issues, containing vitamin D3, calcium, magnesium, K2, strontium, and boron. It is also a multivitamin. As you can learn in chapter 4, amino acid chelates are the best-absorbed forms of minerals; they are primarily what I use in my practice, and are what Bone Support contains. Strontium and calcium compete for binding sites, and thus should be taken at separate times throughout the day. In Bone Support, strontium is taken in the morning, and a calcium blend is taken in the evening.
Compare these nutraceutical options to the most commonly prescribed class of medications for osteoporosis—the bisphosphonates, including Fosamax, Boniva, and Actonel—which prevent the loss of bone mass. These drugs are taken up by your bones and cause the osteoclasts that resorb bone to slow down. They don’t help you to build bone. Gastrointestinal adverse effects are the most common reason that patients discontinue these drugs. You must sit upright for thirty to sixty minutes after ingesting. The medication can lead to gastrointestinal bleeding, increase the risk of esophageal cancer, and increase the risk of fracture. It can also cause low calcium levels (Kennel and Drake 2009). Why is it that dentists ask whether you are on bisphosphonates? Because they need to know how frail your bones may be. Have you ever read the package insert on these drugs? “Side effects include osteonecrosis of the jaw.” This is a disease of the bone where bone tissue dies and the bone collapses. Dentists need to know this before they start drilling into your mouth. As with every decision we make, we must weigh the risks versus the benefits.
Your bones are constantly turning over. It has been said that every ten years you develop a new skeleton. That is an exaggeration, but you get my point. As you get older, this remodeling process slows down, and your bones become weaker. If you freeze the process with bisphosphonates, you are not as effectively building new bone. A dry, dead tree branch will break very easily, and the same is true of your bones. I’ve had several patients who were afraid to take bisphosphonates because they knew someone who experienced adverse events from the medication and wanted safer options.
Bone Support is one of those safer options! Remember that your bones need more than calcium. They need minerals like Magnesium, K2, and strontium. Pitch the soft drinks and carbonated beverages and incorporate weight bearing exercise and optimize your hormone levels! You can learn more about how to optimize hormones in Chapter 6 of my book Your Longevity Blueprint!
Remember, May is Osteoporosis Awareness Month! If you learned something today, please share this blog!
Please give us a review on Facebook or Google!
Thanks for reading! Wellness is Waiting™!
