

I’m not a home builder, I’m a clinician, but I figure that most people know that the foundation of a house is extremely important. Think about it: the foundation has to support the weight of the entire house. If the house is built on a weak or improperly built foundation, the house can eventually crumble. Have you ever seen the kind of devastation that results from a poorly constructed foundation? It’s a costly repair—far more costly than building the foundation right from the start. The same is true for the human body—it must have a healthy foundation on which to build good health. The foundation of your body’s health is your gut, due in part to the fact that 70 to 80 percent of your immune system lives in your gastrointestinal wall.
Many clients have read about the dangers of “leaky gut,” or “gastrointestinal (GI) permeability.” They come to me wanting to fix/heal the condition—they want to strengthen their gastrointestinal foundation.
So, what is leaky gut?
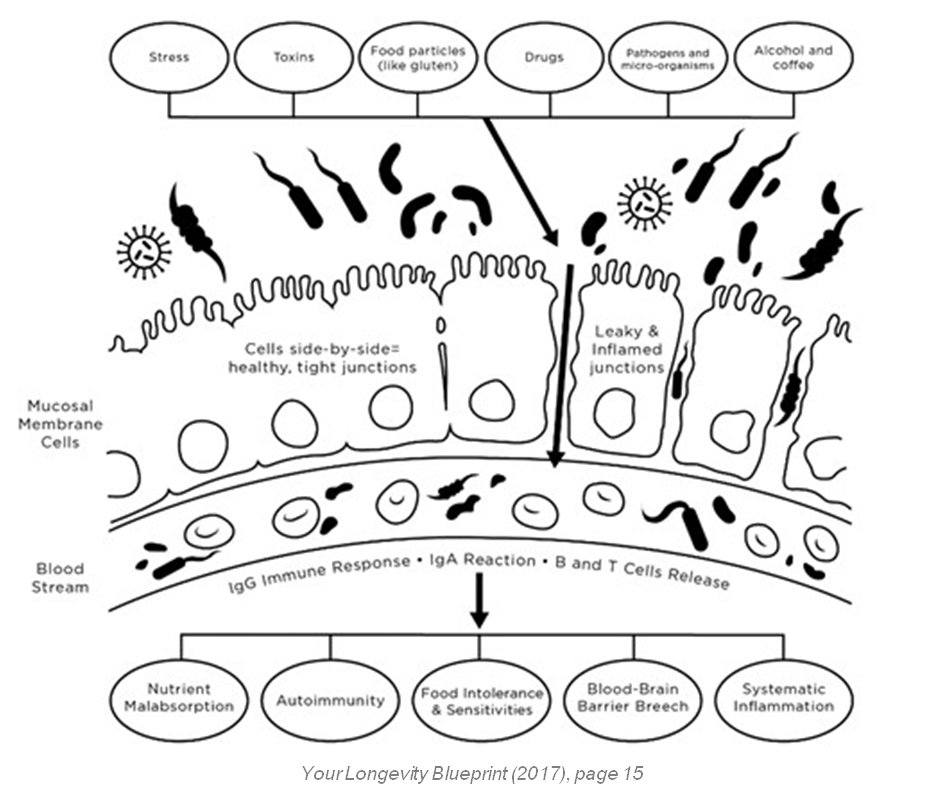
Think of your gut lining as a strong security system. The enterocyte cells that line the gut should be positioned tightly side by side. It’s a little like bricks and mortar in a wall. That lining should permit the absorption of certain nutrients and keep harmful agents out. However, if the layer of cells becomes patchy and gaps begin to develop between cells, harmful substances can leak through the security system.
How does damage to the wall happen? Damage to the gut lining can occur through various stressors, not just psychologic stress, but also medications like antibiotics, which can destroy good gut bacteria-not to mention drinking alcohol and coffee, eating processed and genetically modified foods, and eating foods that cause inflammation (which vary from person to person). Even exposure to germs in your daily environment and incurring stress can damage the gut lining. Then what once looked like brick and mortar now just looks like bricks without mortar. Gaps in the wall develop, allowing proteins that are not supposed to make it through the wall to enter into the blood stream. When that happens, the immune system is triggered to attack them. Even worse, it starts attacking what may have once been a good food for you. The immune system marks those food proteins as bad, and creates antibodies to protect you against them. This can lead to malnourishment, nutritional deficiencies, and even hormonal imbalances, since hormone pathways require these nutrients. And, since your body needs nutrients for the immune cells to function appropriately, it can lead to immune issues. These nutrients are also required for your body to produce energy. In addition, once you have leaky gut, you develop a greater likelihood for food sensitivities. For instance, gluten may have been the biggest trigger for you, but, now that you have leaky gut, the almonds you eat every day are now leaking through the gut barrier into the bloodstream, at which point your body creates antibodies to almonds. Those antibodies will then show up on your food sensitivity testing, even though they weren’t the main problem in the first place. The biggest danger is the inflammatory cascade that can occur and cause various symptoms, which are different for each person.
What are symptoms of leaky gut?
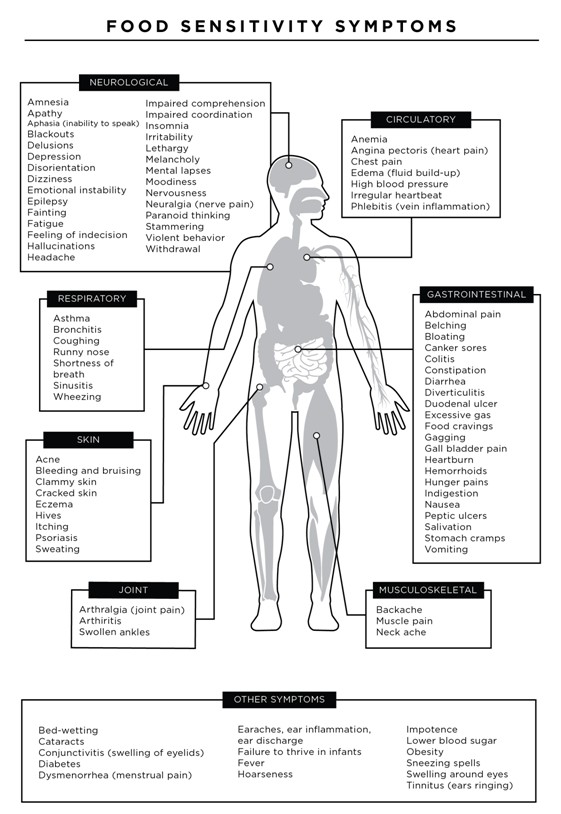
In Chapter 1 of my book, Your Longevity Blueprint, I describe in depth the consequences of leaky gut, one being food sensitivities. The table below shows a long list of symptoms that can occur with food sensitivities and note that these can occur in various organ systems (not just the gut).
For example, what happens on your skin may be a reflection of what is happening in your gut. For instance, I have found that inflammatory conditions like eczema and psoriasis are primarily triggered by food sensitivities or infections. I’ve have patients with acne-like lesions on their head or even hives on their skin who have resolved their symptoms through a change in their diet. Applying a steroid cream or using an antihistamine may help, but that strategy is not getting to the root cause.
Additionally, chronic fatigue, joint pains, fibromyalgia, and even chronic respiratory issues like chronic mucous, congestion, and sinusitis can be caused by food sensitivities (Lord and Bralley 2008). What about chronic ear infections in kids? Could this be a dairy sensitivity? Research has shown that it could (Juntti et al. 1999).
How do you know if you have food sensitivities?
You can try an elimination diet and then monitor how you feel as you reintroduce each food. Alternately, you can test. A true elimination diet removes corn, dairy, eggs, gluten, white sugar, shellfish, soy, beef, pork, processed meats, coffee, tea, and chocolate.
The aim of an elimination diet is to reduce inflammation, identify food triggers, repair leaky gut, and reduce your incoming toxic burden. These foods are avoided for months, and then reintroduced one at a time. The Institute for Functional Medicine (IFM) has a free Comprehensive Elimination Diet Guide available for download to its members.
I commonly see patients who have already tried the elimination diet, and who still can’t quite narrow down what foods are the most problematic for them. If the patient feels gassy, bloated, and has diarrhea after eating pizza, it is difficult to determine whether the problem is the cheese, the gluten, the yeast, the eggs, the garlic in the crust, the tomato sauce, or other toppings. Some patients have told me their allergist has said they have no allergies, but they continue to struggle and know that certain foods cause certain symptoms for them. For instance, I commonly see patients produce a large amount of mucus after having consumed meals containing dairy, such as yogurt, milk, cottage cheese, or ice cream. Even though the patient did not have a full-blown immunoglobulin E (IgE) allergy to dairy, clearly dairy is causing symptoms.
An IgE reaction is the most widely recognized food reaction, one that is so severe that it can cause anaphylactic shock and even death. It is often classified as a Type 1 allergic reaction. By exploring other avenues of testing for different immune reactions to foods, positives are often discovered. In my functional medicine practice, I typically use either immunoglobulin G (IgG), or immunoglobulin A (IgA) blood antibody tests to find these reactions. Most large, functional medicine labs have these food panels available at a reasonable price. And I have found great clinical utility using all of these tests—IgG, IgA, and IgE. There is no perfect test, but the major difference between an immediate IgE and an IgG or IgA reaction is the complicating factor that IgG and IgA reactions can be delayed by hours to even a week (Lord and Bralley 2008). Also, the IgG and IgA tests are not the painful skin-prick tests that many individuals are familiar with, as would be used in an allergist office. IgG and IgA tests are typically done after gathering blood via the venipuncture or fingerstick process. Many foods can be tested at once.
The foods that are commonly tested include:
- egg white and yolk
- milk and cheese
- soy
- gluten grains such as wheat, barley, rye, and oats
- corn
- rice
- shellfish
- various proteins such as beef, chicken, lamb, and pork
- many fruits and vegetables
- coffee
- baker’s and brewer’s yeast
- sugarcane
Expanded panels can be ordered if the patient is on a specific diet, such as vegetarian. Patients do not have to fast for the test, since it is looking an immune response in the blood. However, if the patient is currently on steroids or other immunosuppressants, those should be taken into consideration, since the medication could suppress the immune response. Results could show as potentially false negatives, or as reactions to a lesser degree than they may have shown had the
patient not been on these medications.
Since IgG reactions can take days to manifest, it is also very difficult for individuals to determine what foods are the problem. When I say “reactions,” I am referring to any negative symptoms following consumption of foods. A reaction that takes days to occur is known as a chronic delayed hypersensitivity reaction. That is why testing is so valuable. For instance, if an individual eats a banana on Monday but doesn’t have a headache until Wednesday, bananas may have been ruled out as a culprit when they actually could have been the trigger.
If you’d like to be tested for food sensitivities, please call the Integrative Health and Hormone Clinic and schedule an appointment, 319-363-0033.
In my practice, our health coach reviews patient’s food sensitivities with them in a nutritional consultation to help guide them on what diet changes need to be made based on their personal results. She also walks patients through a comprehensive gut healing protocol – which will be discussed in my next blog.
Read my next blog on how to further heal your leaky gut and get rid of those food sensitivities!

10399 Comments. Leave new